
December 9 2023
8 min read

Sep
Video conferencing emerged as a pivotal tool in patient care amidst digital advancements. Initially popularized in the corporate world for virtual meetings, video conferencing soon found its footing in the medical field. The reasons were manifold.
Firstly, the visual element of video conferencing replicates the face-to-face interaction that is crucial in a doctor-patient relationship. It allows healthcare providers to observe visual cues, such as skin color, facial expressions, and body language, which can be instrumental in diagnosis and treatment.
Secondly, video calls bridges the gap between urban medical facilities and patients in remote or underserved areas. Those who previously had limited access to specialist care due to geographical constraints could now consult with experts from the comfort of their homes.
Moreover, the ongoing global challenges, like the COVID-19 pandemic, underscored the importance of remote consultations. With lockdowns and social distancing norms in place, video conferencing became the lifeline for many, ensuring uninterrupted patient care even in unprecedented times.

One of the most palpable benefits of video conferencing in healthcare is the significant reduction in patient wait times. Traditional in-person consultations often come with the challenges of overbooked schedules, unexpected delays, and prolonged waiting periods. Video conferencing, on the other hand, streamlines the process.
Efficient Scheduling: Digital platforms allow for real-time schedule updates, ensuring that both doctors and patients are aware of any changes or delays.
Minimized Physical Constraints: Without the need for physical travel, patients can log in for their consultation from anywhere, ensuring punctuality.
Optimized Consultation Durations: Digital tools, like pre-consultation forms and health trackers, provide doctors with preliminary information, allowing for more focused consultations.
Geographical barriers have long been a challenge in accessing specialized medical care, especially for patients in remote or underserved areas. Video conferencing shatters these barriers.
Global Reach: Patients can now consult specialists from around the world, ensuring they receive the best possible care irrespective of their location.
Reduced Travel Burdens: Eliminating the need for long-distance travel not only saves time but also reduces the financial and physical strain on patients.
Increased Specialist Availability: Video conferencing allows specialists to cater to a broader patient base, ensuring their expertise benefits a larger community.
Effective communication is the cornerstone of successful medical care. Video conferencing elevates this communication by introducing a visual element that’s often missing in phone consultations.
Visual Diagnosis: Doctors can visually assess symptoms, making diagnosis more accurate.
Personal Connection: Seeing a patient face-to-face, even virtually, strengthens the doctor-patient bond, fostering trust and understanding.
Clarity in Communication: Demonstrations, visual aids, and real-time Q&A sessions during video calls enhance comprehension and ensure patients are well-informed.
The medical field is ever-evolving, and continuous education is paramount. Video conferencing serves as a potent tool for medical professionals to stay updated.
Webinars and Workshops: Specialists from around the world can host or attend sessions, sharing their insights and research without geographical constraints.
Collaborative Learning: Video conferencing facilitates group discussions, case study reviews, and collaborative problem-solving among medical professionals.
Access to Global Medical Libraries: Virtual tours, digital archives, and interactive sessions with global medical libraries ensure professionals have access to a vast reservoir of knowledge.

Telehealth, at its core, is the utilization of electronic information and telecommunication technologies to support long-distance clinical healthcare, patient and professional health-related education, public health, and health administration.
It’s a broad term that encompasses a variety of health care services, including telemedicine, which specifically refers to remote clinical services.
The significance of telehealth lies in its transformative potential:
Accessibility: Telehealth democratizes healthcare, making it accessible to individuals in remote locations or those who face mobility challenges.
Cost-Efficiency: By reducing the need for physical infrastructure and travel, telehealth can lead to significant savings for both healthcare providers and patients.
Flexibility: Telehealth services can be tailored to fit the specific needs of individual patients, ensuring personalized care.
Video conferencing is the linchpin that holds the vast realm of telehealth together. It’s the medium that facilitates real-time, face-to-face interactions, making remote healthcare a tangible reality.
Real-Time Consultations: Video conferencing allows for synchronous medical consultations, where doctors and patients can interact in real-time, ensuring immediate feedback and dynamic discussions.
Visual Examination: While telehealth encompasses various communication modes, including voice calls and text, video conferencing is unique in allowing healthcare professionals to visually assess a patient’s condition.
Multidisciplinary Meetings: Complex medical cases often require the expertise of multiple specialists. Video conferencing facilitates multidisciplinary team meetings, where experts from various fields can collaborate on patient care without being in the same location.

In an era where data breaches are increasingly common, ensuring the privacy and security of patient information during video consultations is paramount. Healthcare institutions must prioritize:
End-to-End Encryption: All video calls should be encrypted, ensuring that unauthorized entities cannot intercept or decipher the data.
HIPAA Compliance: Video conferencing platforms must adhere to the Health Insurance Portability and Accountability Act (HIPAA) standards, safeguarding patient health information.
Multi-Factor Authentication: Implementing additional layers of security, such as OTPs or biometric verification, can prevent unauthorized access.
The efficacy of a video consultation is heavily reliant on the quality of the connection. To ensure seamless interactions:
High-Bandwidth Infrastructure: Healthcare institutions should invest in robust internet infrastructure, ensuring high-speed and stable connections.
Quality Assurance Protocols: Regularly testing the video quality, audio clarity, and connection stability can preempt potential issues.
Backup Connectivity Solutions: Having alternative connectivity options, such as mobile data or secondary ISPs, can be invaluable during unexpected downtimes.

While many medical professionals are adept at in-person consultations, virtual interactions can pose unique challenges. Effective training should encompass:
Platform Familiarity: Ensuring that medical staff are comfortable with the video conferencing tools, understanding features like screen sharing, virtual whiteboards, and session recording.
Virtual Etiquette: Training on maintaining eye contact, ensuring optimal lighting, and minimizing background distractions can enhance the patient experience.
Scenario-Based Training: Simulating various scenarios, from technical glitches to handling emergencies virtually, can prepare staff for real-world challenges.
Virtual consultations inherently differ from in-person interactions. Adapting to this new dynamic requires:
Active Listening: Given the absence of many physical cues, medical professionals must hone their listening skills to understand patient concerns fully.
Clear Communication: Articulating thoughts clearly, avoiding medical jargon, and frequently seeking patient feedback can ensure effective communication.
Building Trust Virtually: Establishing rapport, showing empathy, and consistently following up can foster trust in a virtual environment.

Selecting an appropriate video conferencing platform is the foundation of a successful telehealth initiative. Factors to consider include:
Scalability: The platform should be able to accommodate growth, handling an increasing number of users without compromising performance.
Integration Capabilities: It should seamlessly integrate with existing Electronic Health Record (EHR) systems and other healthcare software.
User-Friendly Interface: A platform that’s intuitive for both healthcare professionals and patients ensures smooth adoption and reduces training needs.
Adherence to health regulations is non-negotiable when implementing video conferencing in healthcare.
HIPAA Compliance: Ensure that the chosen platform adheres to HIPAA standards, safeguarding patient health information.
Data Encryption: All patient data, including video streams, should be encrypted to prevent unauthorized access.
Regular Audits: Conduct periodic audits to ensure ongoing compliance and identify potential areas of improvement.
For video conferencing to be effective, patients need to be active participants.
Educational Workshops: Organize sessions to educate patients about the benefits of video consultations and provide hands-on training.
Accessible Support: Offer dedicated helplines or chat support to assist patients with technical issues or queries related to video consultations.
Feedback Mechanisms: Allow patients to share their experiences and suggestions, fostering a sense of involvement and continuous improvement.
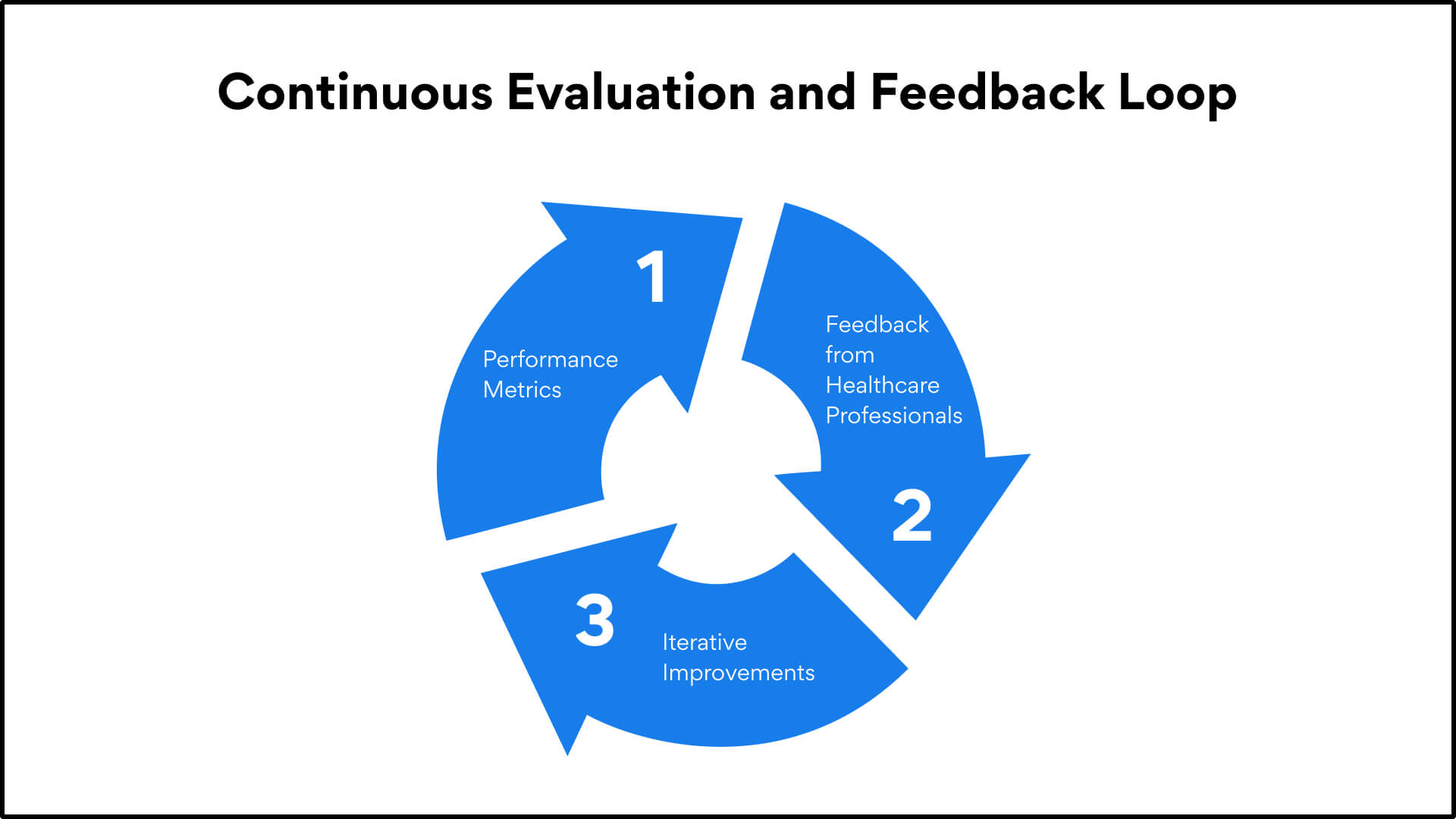
The world of healthcare is dynamic, and so should be the approach to video conferencing.
Performance Metrics: Regularly monitor key performance indicators such as connection stability, video quality, and user satisfaction rates.
Feedback from Healthcare Professionals: Engage doctors, nurses, and other medical staff in providing feedback on the platform’s functionality and areas of potential enhancement.
Iterative Improvements: Based on collected data and feedback, continuously refine and upgrade the video conferencing experience.
The successful implementation of video conferencing in healthcare is a meticulous process that requires careful planning, continuous evaluation, and a patient-centric approach. By adhering to best practices and prioritizing both compliance and user experience, healthcare institutions can harness the full potential of video conferencing, driving improved patient outcomes and operational efficiency.
The integration of video conferencing in healthcare has truly marked a new era in medical practice. This digital shift has bridged geographical gaps, made specialist care more accessible, and improved the overall patient experience.
Video consultations offer immediacy and convenience, not only streamlining medical processes but also empowering patients to take charge of their healthcare journey. The future of healthcare, driven by video conferencing, promises to be more inclusive, collaborative, and innovative.
Trust Confy for top-tier healthcare video conferencing
With Confy’s white label telemedicine, you’re not just getting a video consultation tool; you’re investing in a comprehensive telehealth solution. From seamless video consultations to integrated appointment booking features, both providers and patients have a user-friendly experience. The virtual waiting room feature exemplifies patient-centric design, allowing patients to wait comfortably before their scheduled appointments.
Moreover, our dedication to security ensures that all patient data and consultations remain confidential. In a world where virtual care is becoming the norm, don’t settle for less.

December 9 2023
8 min read

December 4 2023
8 min read

November 30 2023
8 min read

November 22 2023
8 min read