
December 9 2023
8 min read

Aug
The landscape of healthcare delivery is undergoing a profound transformation, driven by the rapid advancement of technology and the need for more efficient and cost-effective solutions.
Telemedicine, once a niche concept, has evolved into a cornerstone of modern healthcare practices. As hospitals and clinics seek ways to streamline operations, improve patient outcomes, and navigate the complexities of healthcare economics, telemedicine has emerged as a powerful tool in their arsenal.
Before tackling the burning question: How does telemedicine reduce costs for hospitals and clinics? Let’s understand the impact of telemedicine.
A Paradigm Shift in Patient-Centric Care
Telemedicine is not merely a technological upgrade but a paradigm shift in how healthcare is delivered and received.
As virtual consultations dismantle the traditional barriers of time and distance, patients gain unprecedented access to medical expertise without needing physical presence.
This empowers patients to seek timely care, mitigating potential complications and reducing the overall strain on healthcare facilities.
To better understand how telemedicine saves money for hospitals and clinics, let’s take a look at the financial challenges they face.
The traditional healthcare model often grapples with skyrocketing operational costs, resource allocation dilemmas, and the escalating burden of preventable readmissions.
The pursuit of high-quality patient care has always been central to healthcare institutions. However, achieving this goal within the constraints of limited resources and escalating costs has become an increasingly intricate challenge.
Hospitals and clinics find themselves in a perpetual balancing act, striving to deliver exceptional care while managing budgets that are stretched to their limits.
One of the most significant financial challenges plaguing healthcare is the high rate of preventable readmissions. Patients discharged after treatment often return due to complications that could have been averted with proper monitoring and timely interventions.
These readmissions not only strain healthcare resources but also inflate costs for both providers and patients.

In the dynamic landscape of modern healthcare, operational efficiency stands as a cornerstone for sustainable growth and cost containment.
Telemedicine, with its technological prowess, emerges as a transformative force in streamlining administrative tasks, optimizing scheduling, and maximizing staff allocation.
Streamlining Administrative Tasks
Administrative burdens often impede the seamless flow of healthcare delivery, consuming valuable time and resources. Telemedicine leverages digital platforms to automate and streamline administrative processes, allowing healthcare professionals to focus more on patient care and less on paperwork.
Optimizing Scheduling for Maximum Utilization
Effective scheduling is pivotal for ensuring that healthcare resources are utilized optimally. Telemedicine introduces a novel dimension by enabling flexible and convenient virtual consultations.
This flexibility translates into reduced patient wait times, increased appointment availability, and a more balanced utilization of healthcare professionals’ schedules.
Staff Allocation and Resource Utilization
Telemedicine transcends geographical boundaries, enabling healthcare providers to allocate their expertise efficiently. Specialists can remotely extend their services to multiple facilities, addressing patient needs across diverse locations. This strategic allocation of staff resources ensures that the right expertise is available to patients, regardless of their physical location.

In the intricate web of healthcare infrastructure, the physical aspects often contribute substantially to operational expenses. Telemedicine emerges as a transformative force, promising significant reductions in the need for extensive physical infrastructure.
Let’s understand the strategic role of telemedicine in minimizing infrastructure costs and providing cost-saving measures in building maintenance, equipment, and facility expansion
Reimagining Healthcare Spaces
Telemedicine redefines the traditional notion of healthcare spaces. By enabling virtual consultations and remote patient monitoring, hospitals and clinics can optimize their existing physical layout.
This paves the way for space utilization efficiency, reducing the demand for expansive waiting areas, examination rooms, and administrative zones.
Equipment Rationalization and Investment
Traditional healthcare delivery often mandates an extensive inventory of medical equipment. Telemedicine introduces a paradigm shift by focusing on technology-driven solutions that require minimal specialized equipment.
This rationalization not only reduces procurement and maintenance expenses but also opens doors for innovative cost-effective alternatives.
Scalable Facility Expansion
Expanding physical healthcare facilities involves substantial financial outlays and intricate planning. Telemedicine’s potential lies in its scalability and ability to cater to a larger patient base without the immediate need for brick-and-mortar expansion.
By effectively leveraging telemedicine technologies, healthcare institutions can accommodate increased patient load without the burden of rapid facility expansion.
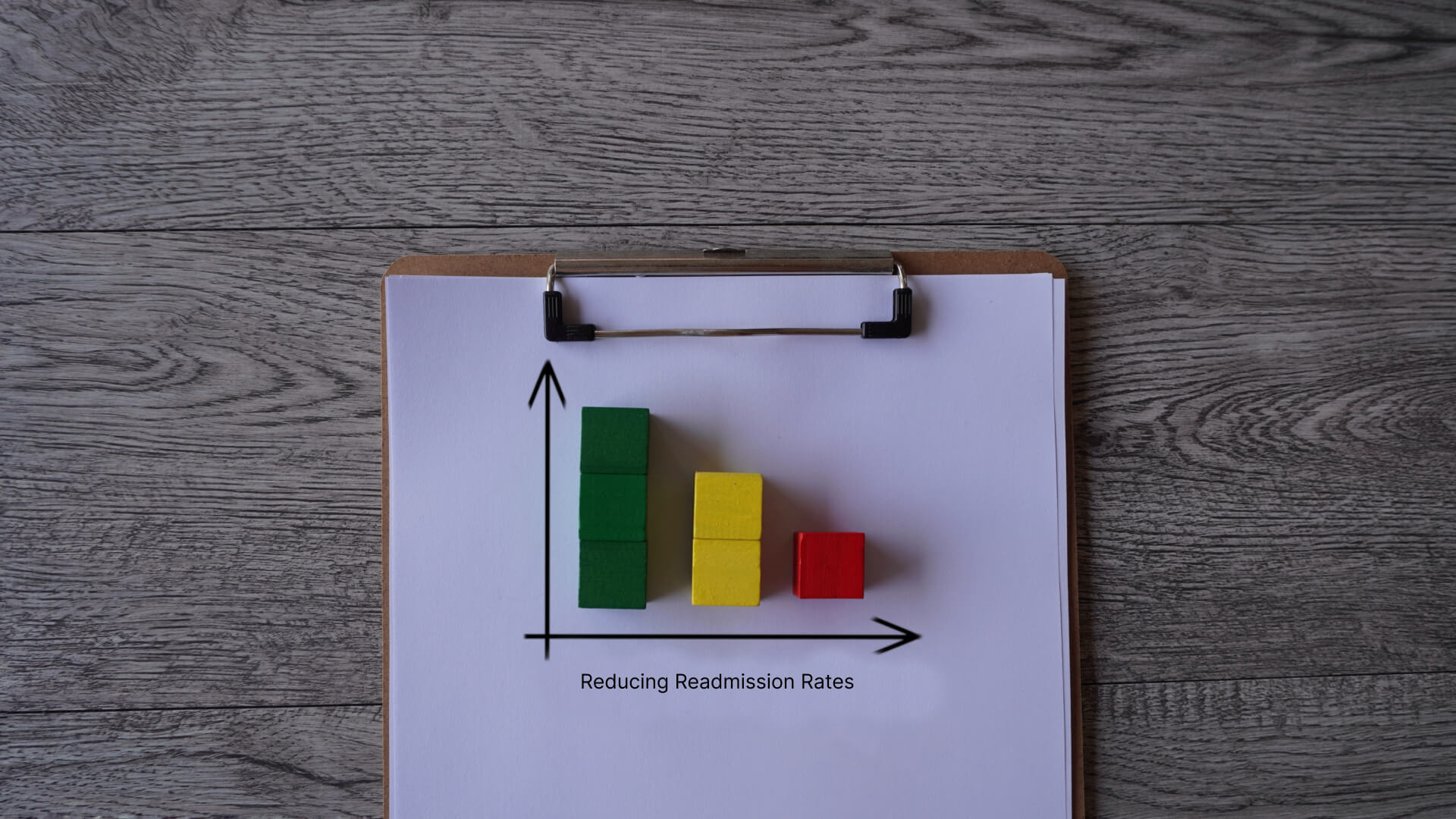
In the pursuit of sustainable and economically viable healthcare, the reduction of preventable readmissions emerges as a critical focal point. Telemedicine, with its transformative capabilities, plays a pivotal role in addressing this challenge by facilitating remote patient monitoring and follow-up care.
Transforming Post-Discharge Care
Telemedicine redefines the landscape of post-discharge care, ushering in a new era of patient engagement and continuity. By harnessing remote patient monitoring technologies, healthcare providers can closely monitor patients’ recovery progress, identify potential complications early, and intervene promptly when necessary.
This proactive approach significantly mitigates the likelihood of preventable readmissions, resulting in substantial cost savings for hospitals and clinics.
Data-Driven Insights for Early Intervention
The integration of telemedicine in post-discharge care introduces a data-rich environment that empowers healthcare professionals with real-time insights into patients’ health statuses.
Continuous monitoring of vital signs, symptoms, and medication adherence allows for informed decision-making and early detection of any deviations from the expected recovery trajectory.
By swiftly addressing emerging issues, telemedicine contributes to a lower incidence of readmissions, thereby reducing the financial strain on healthcare institutions.
Strengthening Patient Empowerment and Compliance
Telemedicine not only enhances clinical oversight but also empowers patients to actively participate in their recovery journeys.
Through virtual consultations and remote monitoring, patients receive personalized guidance and education, enabling them to better manage their health post-discharge.
This increased engagement leads to improved medication adherence, adherence to recommended lifestyle modifications, and heightened awareness of potential warning signs, all of which contribute to reduced readmission rates.
Fostering Collaborative Care Networks
Telemedicine creates a seamless bridge between patients and healthcare providers, fostering a collaborative care ecosystem that extends beyond the confines of hospital walls.
Specialty consultations, follow-up appointments, and even rehabilitation exercises can be conducted remotely, ensuring that patients continue to receive comprehensive care even after leaving the hospital.
This continuity of care minimizes disruptions in the recovery process and decreases the likelihood of readmissions.

Healthcare and finances are closely connected, and telemedicine offers a strategic way to navigate this complexity. Let’s explore how telemedicine reimbursement policies and billing affect revenue and its symbiotic relationship with financial viability.
Timely Reimbursements: A Catalyst for Financial Stability
Telemedicine’s impact on the timely receipt of reimbursements is pivotal for sustaining healthcare operations. Swift reimbursement cycles empower hospitals and clinics to efficiently manage their cash flows, enabling them to invest in advanced medical technologies and optimize patient care.
Pioneering Precision in Billing Accuracy
Billing inaccuracies can have a substantial negative impact on healthcare institutions, leading to a significant loss of revenue and the inefficient allocation of valuable resources
Telemedicine offers a way for precise billing accuracy, as virtual visits are carefully recorded, lowering the risk of billing errors.

As healthcare continues to evolve in the digital age, the boundaries of patient care are extending far beyond the confines of traditional hospital walls. Here, we explore the captivating realm of telemedicine’s capacity to cast a wider net, drawing in a more diverse and expansive patient demographic. Let’s also understand telemedicine’s ability in patient acquisition and market expansion.
A Digital Nexus to the Global Patient Community
Telemedicine serves as a digital nexus, reaching patients irrespective of geographical constraints. This capability is especially profound in rural and underserved areas, where healthcare accessibility has been historically limited. The virtual connection that telemedicine fosters effectively bridges the gap, offering medical expertise to those previously excluded from quality care.
Breaking Down Barriers: Demographic Diversity
Telemedicine’s flexibility and convenience cater to the needs of a wide spectrum of patients. Elderly individuals, individuals with disabilities, and those with busy lifestyles find solace in the accessibility that virtual care brings. This breakdown of barriers ensures that healthcare services transcend age, ability, and circumstance.
Expanding Markets through Virtual Care
Telemedicine augments an institution’s market potential by extending its reach to new patient segments. The ability to cater to diverse medical needs positions healthcare providers to tap into previously untapped markets. This strategic expansion has a cascading effect, driving revenue growth and establishing a robust market presence.
In the intricate dance between modern innovation and conventional healthcare practices , a vital question emerges: does the transformative power of telemedicine translate into tangible financial gains?
Let’s explore economics, dissecting the financial landscape of traditional care and the dynamic realm of telemedicine. Through comprehensive cost analysis, we unveil how telemedicine acts as a beacon for reducing healthcare expenses.
The Ledger of Transportation Savings
Traditional care often mandates patients to embark on journeys that extend beyond the medical encounter itself. These journeys, however necessary, add an additional layer of cost, encompassing transportation expenses, fuel, and time commitments.
Telemedicine, with its virtual consultations, virtually eradicates this component.
The result?
A direct impact on patients’ pockets and a reduction in carbon footprint.
Appointments Unmissed: A Financial Windfall

Missed appointments, a perennial challenge in healthcare, take a toll on both patients and healthcare providers. The traditional paradigm sees patients facing hurdles such as work commitments, transportation challenges, and logistical complexities.
Telemedicine, with its convenience and flexibility, addresses these hurdles head-on.
The outcome?
A substantial reduction in missed appointments casts a ripple effect on the financial stability of healthcare establishments.
A Radical Change in Patient Outcomes
The telemedicine canvas paints a picture of improved patient outcomes through proactive monitoring and timely interventions.
The traditional model, while effective, often falls short in providing the nimble response that evolving medical conditions demand.
Telemedicine’s virtual surveillance equips healthcare teams with real-time data and empowers patients to engage in their well-being.
This translates to a reduction in hospital readmissions, a critical financial consideration for healthcare institutions.
So, “How does telemedicine reduce costs for hospitals and clinics?” The answer is simple yet powerful: by redefining efficiency, streamlining operations, and unleashing the potential of technology to drive down expenses without compromising care quality.
With telemedicine, the future isn’t just bright – it’s healthier, wealthier, and brimming with possibilities. The healthcare world has seen its fair share of revolutions, but telemedicine stands as a beacon of hope, proving that the greatest breakthroughs often come from thinking outside the box – or, in this case, outside the hospital walls!
Level Up Your Healthcare Game with Confy’s White Label Telemedicine App
Ready to supercharge your healthcare strategy and make life easier for your staff, your budget, and your patients? Picture this: Confy’s awesome white label telemedicine platform swoops in to save the day. No more headaches with paperwork – we’re talking streamlined everything.
So, why wait? Reach out to us now and let’s chat about how Confy’s white label telemedicine solution can totally transform your healthcare game. Get ready to high-five better patient outcomes, mega cost savings, and a healthcare vibe that knows absolutely no bounds.
Q1: Does telemedicine compromise the quality of care?
A: No! Telemedicine empowers doctors to provide personalized care, answer questions, and monitor progress, just as they would during an in-person visit.
Q2: What about patients who aren’t tech-savvy?
A: Telemedicine platforms are designed with user-friendliness in mind, and most patients find them a breeze to navigate. Hospitals often provide support to ensure everyone receives the care they need.
Q3: Can telemedicine handle emergencies?
A: While telemedicine works wonders in many scenarios, it’s not a replacement for urgent care. In emergencies, heading to the nearest hospital remains the golden rule.

December 9 2023
8 min read

December 4 2023
8 min read

November 30 2023
8 min read

November 22 2023
8 min read