
December 9 2023
8 min read
Oct
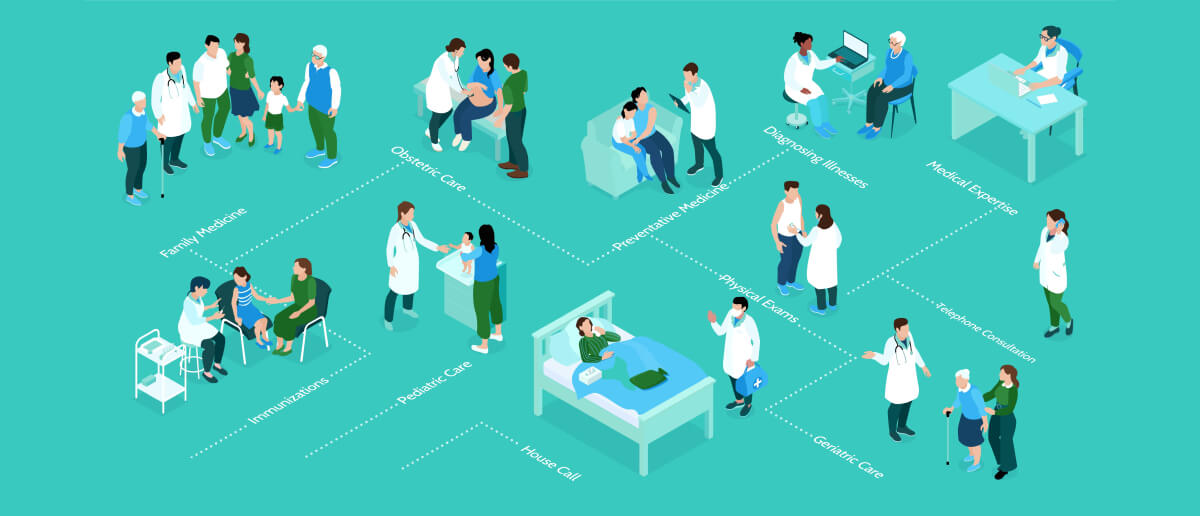
Patient Flow Management (PFM) is the coordinated, systematic approach taken by healthcare institutions to ensure that each patient’s journey—from initial entry to discharge—is smooth, timely, and efficient. At its core, PFM harmonizes the operational aspects of care delivery with the clinical needs of patients. The ultimate goal is to enhance patient satisfaction, reduce healthcare costs, and ensure optimal utilization of resources.
Efficiency is more than just a buzzword when it comes to the healthcare sector. Let’s break down its significance:
Improved Patient Experience: The quicker a patient proceeds through various stages of care, the better their overall experience. Delays often lead to increased anxiety and dissatisfaction.
Optimal Resource Utilization: Efficient patient flow means resources like beds, equipment, and staff are used judiciously. This prevents unnecessary expenses and ensures readiness for emergencies.
Reduced Clinical Risks: A patient left waiting might experience a deterioration in their condition. Efficient flow minimizes these potentially hazardous waiting times.
Enhanced Staff Morale: When the system is streamlined, healthcare professionals can focus on patient care rather than administrative hurdles, bolstering morale and job satisfaction.
Over the years, healthcare professionals have observed recurring bottlenecks that can hamstring the patient journey:
Inefficient Bed Management: Insufficient tracking of bed occupancy can lead to significant wait times, especially in emergency scenarios.
Paper-Based Systems: Manual paperwork is prone to errors and misplacements, causing delays in treatment and discharge processes.
Limited Communication Channels: Lack of efficient inter-departmental communication can lead to delayed test results, misinformed staff, and prolonged wait times.
Mismatched Skill Deployment: Without a proper system, staff might be deployed in areas they’re not specialized in, leading to inefficiencies.
Unpredictable Patient Influx: Sudden increases in patient intake, such as during epidemics or accidents, can overwhelm traditional systems that lack flexibility.

The power of data in modern healthcare cannot be understated. By leveraging accurate, real-time data, you can do the following:
Informed Choices: Clinicians can make decisions that reflect the current status of the healthcare setting, rather than relying on outdated or anecdotal evidence.
Performance Analysis: Regular monitoring and evaluation of key performance indicators (KPIs) related to patient flow can shed light on areas that need improvement.
Predictive Capabilities: Advanced data analytics allow institutions to forecast patient intake, optimizing resources ahead of time.
A static system is a failing system. Embracing change through:
Regular Audits: Periodically assessing processes and procedures to identify inefficiencies.
Feedback Mechanisms: Encouraging staff, patients, and other stakeholders to voice concerns and provide input can highlight potential improvement areas.
Adaptability: Being open to altering workflows, incorporating new technologies, or retraining staff as needed ensures the system remains contemporary and efficient.

The patient should always be at the center of any healthcare strategy. Here’s why:
Enhanced Experience: A system tailored to patient needs invariably leads to better care outcomes and higher satisfaction levels.
Reduced Wait Times: By focusing on the patient, redundancies and unnecessary procedures can be eliminated, leading to quicker care delivery.
Holistic Health: A patient-centric approach often considers the overall well-being of the patient, rather than just treating specific ailments.
Clear, concise communication is the linchpin of efficient patient flow. Its pivotal roles include:
Inter-departmental Coordination: Ensuring different departments work harmoniously can drastically reduce wait times and improve the allocation of resources.
Patient Trust: Keeping patients informed about their care journey, expected wait times, and procedures can foster trust and compliance.
Reducing Errors: Effective communication minimizes misunderstandings, which can often lead to clinical errors or procedural inefficiencies.
Mastering the art of patient flow management hinges on these core principles. They form the backbone of an efficient, patient-friendly, and cost-effective healthcare system. Institutions that embody these principles not only deliver superior care but also position themselves favorably in an increasingly competitive healthcare landscape.

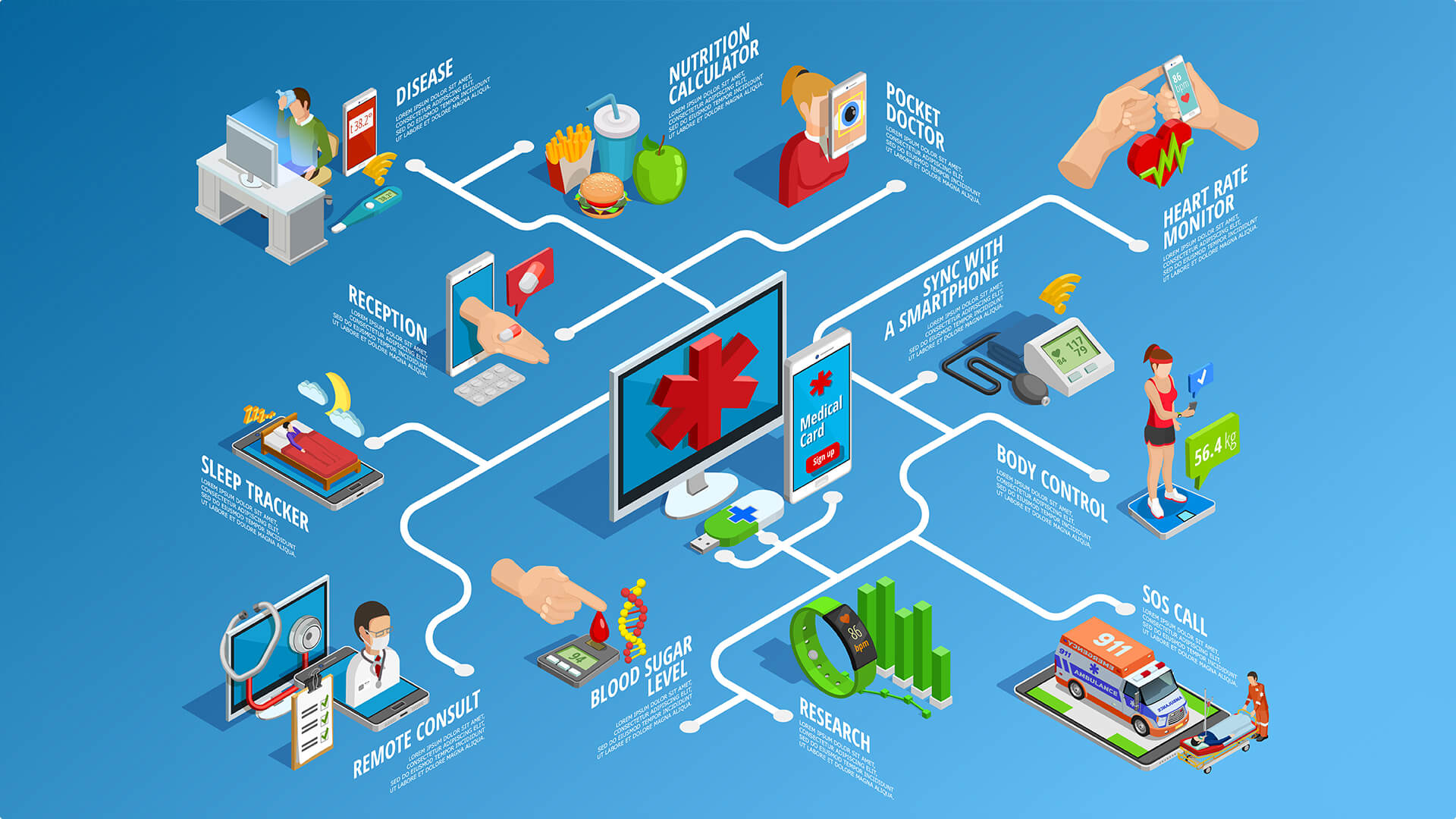
In today’s healthcare, it’s crucial to have a wide range of advanced tools and technology. This extensive toolkit not only optimizes patient flow but also enhances the overall quality of care. Let’s understand the cutting-edge tech that’s reshaping healthcare.
The heart and soul of any healthcare infrastructure is its ability to keep accurate, up-to-date records. Modern EHRs, a considerable upgrade from traditional paper records, provide:
Instant Access: Clinicians can instantly access comprehensive patient histories, ensuring informed decisions.
Interoperability: EHRs can communicate across departments and even between different healthcare institutions.
Efficiency: Automating various administrative tasks, such as billing, directly from the patient’s records.
Time, in healthcare, equates to lives. Knowing where a patient is at any given moment offers several benefits:
Reduced Wait Times: Minimize patient wait times by analyzing and forecasting resource availability in real-time.
Streamlined Movement: Monitor patient movements, ensuring efficient transfers between departments or rooms.
Safety: Swiftly identify and respond to unexpected patient movements or changes in condition.

The global pandemic underscored the need for remote healthcare. Telemedicine tools are now integral to patient flow:
Remote Consultations: Address minor concerns or conduct follow-up consultations without physical visits.
Expanded Reach: Offer healthcare services to remote or underserved locations.
Triage: Pre-assess patients before they arrive, ensuring resources are allocated appropriately.
Marrying healthcare with artificial intelligence (AI) and analytics spells a future where predictions save lives:
Demand Forecasting: Predict patient inflow based on historical data and external factors, allowing for resource optimization.
Personalized Care: AI can analyze a patient’s records and suggest tailored care pathways.
Operational Efficiency: Predictive analytics can suggest tweaks in operational procedures to boost efficiency.
The significance of these technologies is not just in their individual capabilities, but in how they interplay. A well-integrated system forms the backbone of a 21st-century healthcare institution poised for success.
In healthcare, achieving a smooth patient flow relies on modern tools and the effective use of best practices. Let’s explore these proven methods to turn disorder into a well-organized process.
In healthcare, achieving a smooth patient flow relies on modern tools and the effective use of best practices. Let’s explore these proven methods to turn disorder into a well-organized process.
Ensuring timely care for critical patients is the cornerstone of effective flow management. The best approaches include:
Triage Protocols: Implement rapid assessment strategies to categorize patients based on urgency.
Dedicated Resources: Reserve specific beds and equipment exclusively for high-priority cases.
Streamlined Processes: Minimize administrative hurdles for critical care admissions.
A centralized hub, a singular point of entry, can be a game-changer:
Unified Data: One-stop data entry reduces redundancy and errors.
Efficiency: Minimize patient wait times by swiftly allocating resources.
Better Oversight: A centralized view aids in real-time decision-making.

An orchestra is only as good as its conductor. Scheduling and bed management are the conductors of this symphony:
Dynamic Scheduling: Adjust schedules in real-time based on patient inflow and resource availability.
Bed Turnover Protocols: Implement practices like rapid clean-up and setup for swift bed turnovers.
Visibility: Utilize digital dashboards to offer a real-time view of bed availability across departments.
Human resources are the most valuable asset. Deploying them effectively ensures a smoother flow:
Role Clarity: Clearly define roles to avoid overlaps and ensure every task is catered to.
Cross-Training: Equip staff with skills to handle multiple tasks, ensuring flexibility.
Shift Management: Adopt software solutions to create efficient shift rotations, minimizing burnout and ensuring round-the-clock care.

Improving patient flow comes with its challenges. Despite its potential for transformation, the path is filled with complexities. Let’s explore the main obstacles and find solutions to understand the full potential of patient flow.
Healthcare’s intricate web of regulations can be daunting. But with vigilance, it’s navigable.
Stay Updated: Regularly review legislative updates relevant to patient management.
Consultancy: Engage legal experts familiar with healthcare compliance.
Automated Audits: Implement systems that periodically ensure compliance with all standards.
Change, even for the better, can be unsettling.
Inclusive Training: Offer comprehensive training programs on new processes and tools.
Feedback Loop: Cultivate a culture where staff feedback is valued and integrated.
Phased Implementation: Introduce changes incrementally to allow gradual adaptation.

In the age of data breaches, patient data sanctity is paramount.
Advanced Encryption: Use top-tier encryption for data both at rest and in transit.
Regular Audits: Schedule periodic security assessments to identify vulnerabilities.
Staff Training: Ensure all personnel are educated on data handling best practices.
The only constant in technology is change.
Scalable Systems: Choose platforms that are modular and can evolve with advancing technology.
Continuous Learning: Encourage staff to engage in ongoing tech education.
Technology Partnerships: Collaborate with tech vendors that prioritize updates in line with industry innovations.
In summary, patient flow management is not just a passing fad; it’s a powerful driver shaping the future of healthcare. As we approach groundbreaking changes, the healthcare community is called upon to lead this dynamic initiative, guaranteeing a future where care is prompt, effective, and focused entirely on the patient.

December 9 2023
8 min read

December 4 2023
8 min read

November 30 2023
8 min read

November 22 2023
8 min read