Telemedicine can be defined as the practice of using Information Communication Technology (ICT) to facilitate remote healthcare service wherein patients can virtually connect with their doctors and receive the same medical support that they get during an in-person visit, such as:
In the most literal sense, it implies “healing at a distance”. This is the simplest definition, popularized by the World Health Organization (WHO).
The term ‘Telemedicine’ is a Portmanteau word which originated from the Greek word ‘Tele’ meaning distance and the Latin word ‘Meden’ meaning to heal. It is still not listed as an English word by the Oxford dictionary but is used nonetheless.
The ambiguity surrounding all these modern health terminology arises from the fact that even top-tier medical organizations like the World Health Organization (WHO) are often guilty of using these terms synonymously even though there exists a bit of contextual difference. So naturally, anyone new to the concept will have plenty of questions like:
What is the difference between telehealth and telemedicine?
What is the difference between telemedicine and e-Health?
What is m-Health?
The doubts are endless, but the solution? One!
Our team at Confy conducted extensive research to untangle this mystery once and for all.
Truth be told, the medical world is yet undecided on whether to identify the two separately or not. Organizations like the American Medical Association (AMA) believe that, “the definition of both have continued to evolve, and there is no consensus on segregating either of the two terms.”
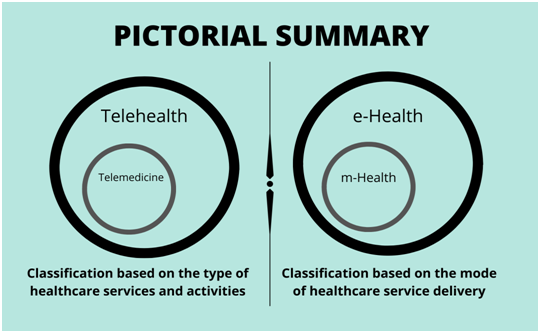
Other institutions like The International Organization for Standardization (ISO) consider Telemedicine to be a subset of Telehealth and therefore, prefer to give separate definitions.
In the widely-accepted sense─
Telemedicine is restricted to the delivery of remote clinical health services which involve aspects of only direct patient care
Telehealth offers a wider scope where health information technology (HIT) can be used beyond clinical causes, for non-clinical services as well; such as, distance medical education, training of healthcare professionals, administrative meetings, etc. that work overall to improve the entire healthcare sector.
Another alternate terminology that World Health Organization sometimes uses is ‘Telematics’ which it defines as ‘a composite term for both or any health-related activities carried out over distance by means of information communication technologies.’
If you haven’t already guessed what ‘e’ and ‘m’ stand for, let us say it out loud- ‘electronic-Health’ and ‘mobile-Health’. So what’s the difference?
You got that right again!
mHealth refers to the types of wellness services that are delivered only through mobile applications via smartphones and tablets. According to the WHO Global Observatory for e-Health series - Volume 3, m-Health capitalizes mobile features like voice messages, short messaging service (SMS), Bluetooth technology, general packet radio service (GPRS), global positioning system (GPS), etc.
On the other hand, e-Health is the umbrella term that encompasses every form of telemedicine and telehealth service, and that includes m-Health as well.
If you are looking for the origins of telemedicine now, chances are that you came to know about this futuristic domain of healthcare as a consequence of the global Covid-19 pandemic. But did you know that back in 2006, we had already crossed the hundred-year milestone already
Yes, you heard it right — a ‘CENTURY’!
The term 'Telemedicine' was coined by Thomas Bird in the 1970s, but its modern use dates back to 1906. Its origins trace even earlier to the 1800s, utilizing telephonic communication to bridge geographical healthcare gaps. An instance in 1879 involved a doctor diagnosing a child over the telephone, as published in The Lancet.
Over time and via technological advancements, the concept has evolved into an advanced virtual care system. Officially, 1906 marks its inception to simplify historical context.
1906 A Dutch physiologist named Willem Einthoven creates the first-ever electrocardiogram (ECG) using a string galvanometer and telephone wires. Using that, he records the electro-cardiac signals of patients staying in a hospital 1.5 kilometers away from his laboratory in Leiden. He later received the 1924 Nobel Prize for his invention.
1920 Doctors in Norway start to frequently diagnose and treat sick ship crew members on voyage via radio communication.
1925 In the February issue of Science and Invention magazine, Hugo Gernsback, a radio pioneer publishes an article on the possibility of a futuristic telemedicine technology called ‘Teledactyl’ where he explains how, in the future, doctors will be able to feel their patients from a remote location using radio and robotic arms.
1959 A two-way closed-circuit microwave television connects doctors and medical students at Nebraska Psychiatric Institute with the patients of Norfolk State Hospital to facilitate video-consultations, research, and training.
1967 Thomas Bird and his team provide treatment to more than a thousand ailing airport employees and travelers via an audio-visual microwave circuit between the Massachusetts General Hospital in Boston and the Logan Airport (roughly 3 miles apart).
1973 NASA, Lockheed Missiles and Space Corporation, Indian Health Service (IHS), the US Department of Health, Education and Welfare, and Papago Nation (now the Tohono O’odham Indian Nation) joins hands to carry out a large-scale telemedicine project STARPAHC (Space Technology Applied to Rural Papago Advanced Health Care). Under this pilot project, a remote clinic in the village of Santa Rosa, a mobile health unit, a referral center at the IHS hospital in Phoenix, and a control center in the IHS hospital on the Papago reservation all get connected using a two-way microwave, telephone, and VHS radio communication.
The 2000s The invention of the World Wide Web in 1989 opens new doors for technological adventures and paves the way for health IT. Telemedicine begins to transcend laboratory boundaries and becomes a go-to solution for healthcare cases with distance as a barrier. For example- treatment of prison inmates, healthcare for people living in rural areas, elderly patient’s health monitoring at old age homes, etc.
There are three types of telemedicine or telehealth services based on the modalities of communication.
Real-time Telehealth, also known as synchronous telemedicine, entails live video-chat for patients and providers. This method enables virtual connections through two-way audio-visual platforms, delivering comparable medical services to in-person visits.
This is commonly used for-
While phone consultations and video calls through apps like Skype, Zoom, or FaceTime are essentially real-time telemedicine, they might not always be legally recognized as so. Video conferencing procedures must adhere to HIPAA compliance for patient privacy. Hence, using authorized platforms like Confy is advisable.
Store and forward is the second type of telemedicine which involves the electronic transmission of medical information such as-
Needless to say, this type of telemedicine is designed for lower priority medical attention like the assessment of medical reports, non-urgent diagnosis, etc.
One major advantage of store and forward telemedicine is its independence from requiring simultaneous attention from all involved parties, unlike synchronous methods. Patients can securely upload medical information, allowing busy healthcare professionals to review it at their convenience. Asynchronous approaches are also beneficial for individuals in varying time zones.
Store and forward practice is best suited for healthcare sectors like radiology, dermatology, and ophthalmology.
Remote Patient Monitoring, also known as telemonitoring, is the distance monitoring of a patient’s vital signs like
Unlike the other two types of telemedicine, remote patient monitoring is beneficial to record and assess the improvement or deterioration of health over a longer period. Remote patient monitoring (RPM) is therefore very well-suited for chronic illnesses like diabetes, hypertension, asthma, cancer, etc.
For a better understanding of how it works in different ways, take a look at this interesting video:
What is telemedicine best suited for? Contrary to the popular belief that it can be used only for primary care, it finds application across numerous medical specialties such as:
According to a study by the American Medical Association, telemedicine has a varied degree of usage across different segments of healthcare. While some medical specialties use the technology for telemedicine to extend patient-provider interaction, others rely on telehealth more for Provider-Provider interaction.
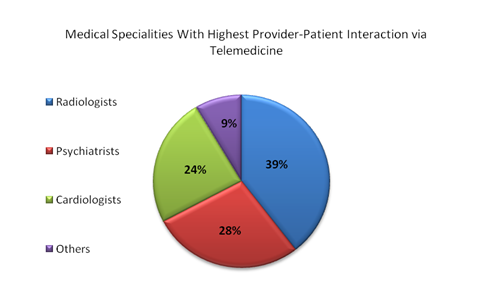
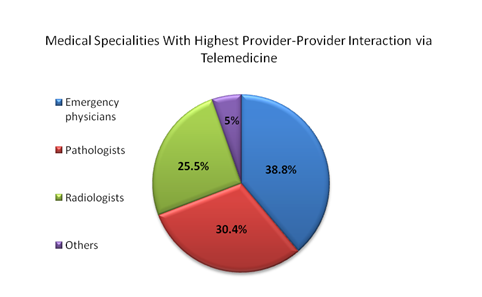
The following are some of the top medical specialties where telemedicine is the preferred alternative:
Dermatological problems can range from just a harmless mole to symptoms of more serious conditions like skin cancer. However, an initial prognosis does not always require a face-to-face visit to the doctor’s clinic. Also, certain infections (like ringworm or tinea infections) pose the threat of being contagious. In such cases, telemedicine can be used to reduce the spreading of infections and also save unnecessary commute time.
As you might have already noticed in our brief timeline of telehealth, cardiology was one of the medical specialties pioneering in telemedicine. Telemedicine resources have frequently used this segment of healthcare to monitor and analyze patients’ cardio-vascular signals from wearable devices or bodily implants. Tele-cardiology is quickly expanding its applications in form of the highly cutting-edge practice of tele-stenting.
The use of telemedicine for behavioral health is something that often doesn’t get the attention than it deserves. Even today, millions of people are silently suffering from mental anxiety, depression, or trauma. Yet, many of them simply avoid checking into a therapeutic clinic in fear of being spotted by an acquaintance and being labeled ‘crazy’. Tele-therapy offers the necessary privacy in this regard.
If there is one medical field that reaps the maximum benefits of telemedicine, it is radiology. Radiology heavily relies on medical imaging and sharing of medical information across a network of multiple healthcare professionals whose schedules might be difficult to co-ordinate. The store and forward type of telehealth, therefore, finds immense importance in this medical specialty.
This technology for can be applied for three broad purposes- (1) Patient care (2) Medical Education (3) Research
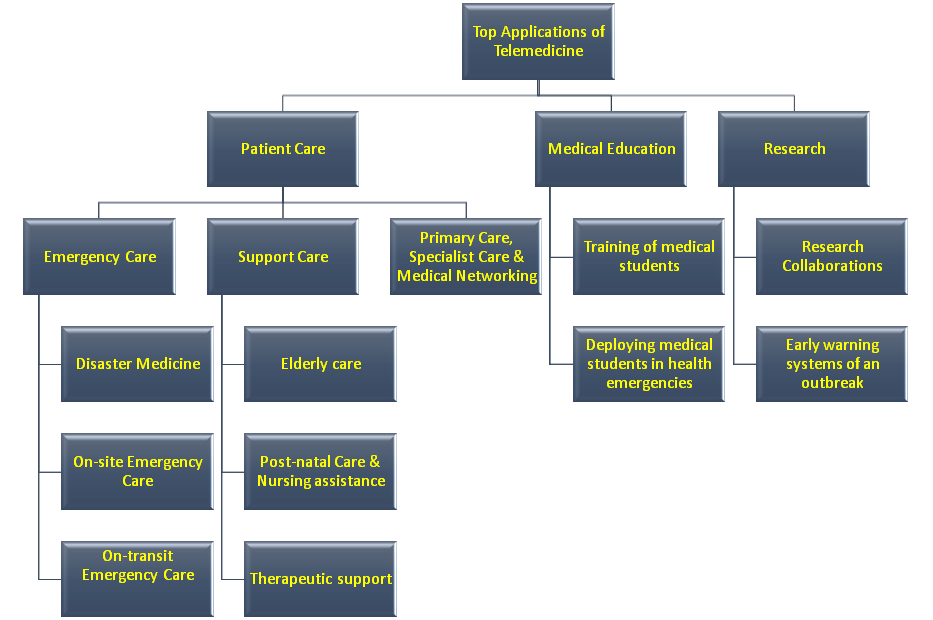
Modern telemedicine is most widely for patient care, be it for emergency purposes or for lifestyle support or even home-monitoring.
Telemedicine in primary care has been most widely used to manage chronic diseases, thanks to home-monitoring devices like a pulse oximeter, smart clothes with ECG devices, blood pressure monitors, glucometers, step-counters, etc. According to research, telehealth monitoring reduced hospital admission rates in patients suffering from the chronic obstructive pulmonary disease (COPD).
In many places, particularly in rural areas, where primary care itself can be a rarity, specialist care is nothing short of a distant dream. There are still many remote villages in the world which have only one all-purpose clinic with just a few healthcare professionals (often having only rudimentary medical knowledge!). According to an article by The Atlantic, nearly 6000 places in the U.S. are in dire need of more primary care doctors. Roughly, one-fifth of American population thrives in rural regions, yet, only one-tenth of medical practitioners work there. Hence, telemedicine and telehealth can play a pivotal role in improving the overall health of the world’s rural population by virtual medical networking.
Telehealth services have found groundbreaking results for emergency care.
According to Our World in Data, an average of 60000 lives are lost each year globally due to natural disasters like floods, earthquakes, hurricanes, landslides, wildfires, etc.
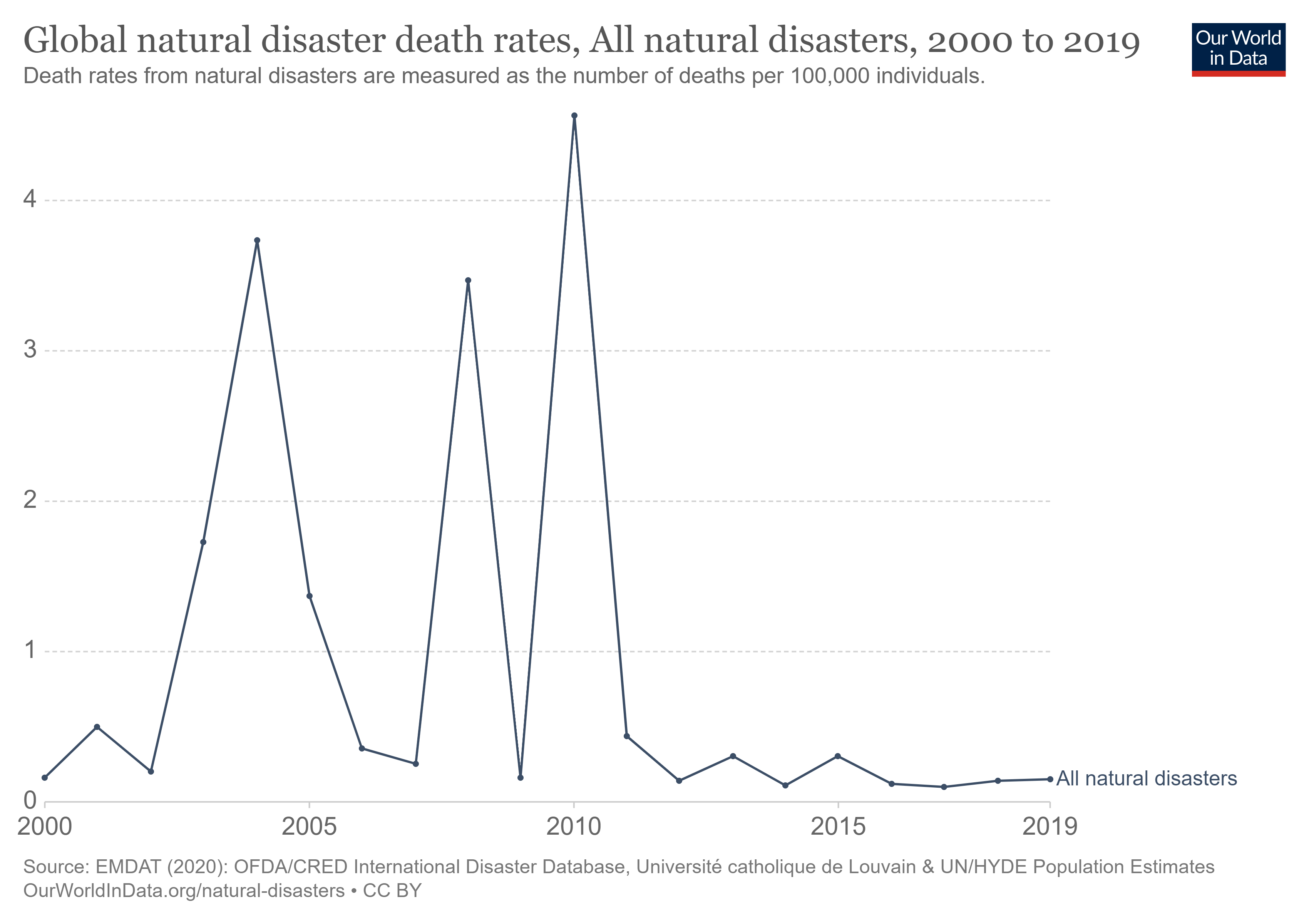
A significant percentage of these deaths is caused due to the inaccessibility of proper medical treatment in the aftermath of the disaster.
In cases where hospitals are critically damaged, the patient-to-doctor ratio is overwhelmingly poor, and physical communication is impossible, telemedicine can take the center stage. Using video-conferencing, paramedics, or local volunteers on the spot can take specialists’ help for temporary first aids and minor procedures, and thereby save lives.
This, in fact, been successfully applied several times to provide emergency response to natural disasters. For example, NASA played a pivotal role to extend disaster aid via telehealth technology during the catastrophic earthquake of 1985 in Mexico City.
In the United States, accidents are the third leading cause of death.
Accidents can occur on the road, in schools and offices, or even at home. Most cases of severe accidents (like road accidents) hardly ever permit the time for the victim to be transferred to a hospital or even wait for an ambulance. Telemedicine services can play vital life-changing roles in such situations.
It plays a crucial role in emergency situations, like cardiac arrest. Often, we recognize the signs of cardiac arrest but lack clarity on the appropriate response. Incorrect CPR attempts can exacerbate the situation. In this technological age, a straightforward software call can connect us with trained healthcare professionals. They can remotely guide us through the correct CPR procedures, effectively reviving the patient.
The very objective of telemedicine is to ensure on-demand and optimized access to healthcare. Although paramedics or emergency medical technicians (EMTs) are somewhat skilled at handling critical situations, they might need specialist guidance from time-to-time. This becomes especially important while the ambulance shuttle time to the hospital is too long (for traffic or distance).
Support care is the continuous care delivery achieved via telemedicine solutions, something that used to be a rather difficult task in the earlier days.
Traveling long distances to a clinic and then waiting for hours to see the doctor is a common ordeal that we have all been through at some point. Many people often avoid or cancel consultation appointments due to these factors. The result disadvantages both the parties involved. The clinics and hospitals suffer huge losses due to patient no-shows. On the other hand, the patients ultimately end up aggravating their health conditions.
But, the experience of an in-person visit (often for minor health issues or routine check-ups) can be particularly painful for the ailing elderly patients. It is indeed a fact that older generations may initially find the technology for telemedicine to be a little difficult to operate, nevertheless, if you ask an elder patient to choose between traveling to the doctor’s chamber and learning a few simple steps to operate a telemedicine app, the answer wouldn’t be a hard guess!
Aside from allowing the comfort of home, telemedicine technologies can also help senior patients living alone or in assisted living facilities to manage their medications. Some Telemedicine application features that can commit to medication management are-
The handling of a newborn baby can be an intricate task, especially for the first-time or adoptive parents. Many parents would agree to have had countless experiences of running to the pediatrician in their night pajamas. Well, babies love to wake you up in the middle of the night! Jokes apart, this can be quite a terrifying experience; especially if one lives away from the cities.
But, nowadays, with the help of a simple video conference from home, parents can seek routine advice from the doctors. Pediatricians can use a platform to observe a baby’s movements to trace anomalies (especially if the baby is premature or has health risks). Nurses can also train parents in swaddling techniques, pacifying tricks, feeding techniques, etc.
As mentioned earlier, (before in the list of telemedicine medical specialties), the remarkably higher degree of privacy in a virtual doctor visit makes telemedicine so beneficial for patients with therapeutic needs. People with mental stress, drug addicts, soldiers suffering from PTSD, and even dysfunctional family members can heal privately.
Telemedicine solutions can also be used to provide remote training and education to medical students.
Telehealth is not made up of a single motif. Although it simplifies healthcare, the solution itself is an advanced potpourri of different disciplines and skill sets- medical, technical, technological as well as legal. So, all the participants (hospitals, doctors, nurses, patients, developers, governments, etc.) are required to have a holistic understanding of the system and their role within it. Therefore, training is essential.
In case of crises like the ongoing Covid19 pandemic, Telemedicine can also act as a secure tool to maintain continuity in medical training and education through virtual anatomy laboratories, simulations, asynchronous course lectures, etc.
A survey by the Liaison Committee on Medical Education (LCME) found that almost half of the medical schools in the United States have implemented telemedicine training in the clerkship phase of their curriculum while about a quarter of them have introduced the same in the pre-clinical phase.
The healthcare landscape is expected to change drastically in the aftermath of the pandemic. With lessons learned, many more medical institutions all across the world will incorporate training in their curricula so that the medical world is prepared well in advance to counter any future global health crisis.
Medical students can use Telemedicine to practice emergency response, disaster response remotely without disrupting the actual response or relief works.
In case of critical situations with a manpower shortage, medical students can help the professionals in peripheral activities like maintaining pharmacy logistics, patient electronic health records, etc.
This practice allows future doctors and nurses to have real-world experience before landing on the actual scene of medical emergencies.
The technology for telemedicine technology can contribute immensely to the field of research.
As mentioned before, Telemedicine eases the process of communication by overcoming barriers of geography and temporal synchrony. Medical students, researchers, healthcare professionals, administrations can all use telemedicine platforms to collaborate and share their expertise and skills for higher efficacy remotely and securely resulting in faster outcomes.
Another advantage of telemedicine for research purposes is its capability for continuous and automated incident analysis. In future endeavors, leveraging regulations and security protocols, artificial intelligence can be integrated into intelligent telehealth software solutions. This would alert the medical community when the system detects early signs of a disease outbreak.
Likewise, the features can serve the purpose of pharmacovigilance for new market-released drugs.
Healthcare is a basic human right.
Yet, in a time when technological advancements in the medical world have progressed to unimaginable heights, access to basic medical care is still a tall order for many of those who are economically weak or reside in remote and rural areas:
Telemedicine in healthcare can bring the whole world inside a small laptop, tablet, or smartphone. Virtual visits are particularly beneficial for-
Medicare spends roughly $26 billion on hospital readmissions, of which roughly $17 billion is believed to be avoidable. That is why the Centers for Medicare & Medicaid Services (CMS) introduced the Hospital Readmissions Reduction Program (HRRP) in 2012. Under this program, hospitals are financially penalized if readmission rates (re-admitting within 30-days of discharge) are higher.
Various Telehealth programs across the U.S. have shown that the rates can be significantly cut down by proper home-monitoring of patients’ vitals and constant engagement with providers with sufficient follow-up consultations and patient education.
One such glaring example can be the telemedicine program implemented by the University of Virginia Medical Center which showed a 10% reduction in hospital readmission rates.
Telemedicine visits enhance patient engagement. An email newsletter or mobile notification from a telemedicine app reminding the patients about an upcoming appointment can relieve busy working patients from the stress of constant presence of mind for a trivial matter. This, coupled with the access to better medical care from the comfort of home, has an overwhelming level of positive effect in terms of patient satisfaction and trust-building among patients and providers.
Many have a fear that the cost of telemedicine and telehealth will be very high. However, the reality is more optimistic.
A common misconception is that telemedicine benefits only the patients. But, in fact, there are several benefits of telemedicine for clinics and hospitals as well.
In the United States, the healthcare sector incurs an annual loss burden of $150 billion only from patient no-shows. A patient no-show happens when a patient neither shows up for an appointment nor cancels it. And this does not necessarily happen only in cases of consultation appointments.
Some common examples of patient no-shows include- absence from follow-up appointments and diagnostic check-ups (like mammography, radiography, MRI scan), surgery postponement, ambulance service cancellation, etc.
Patient no-shows have tremendous negative impacts in terms of resource utilization, wastage of useful time slots, increased wait-time for other patients, and an overall financial loss.
Some of the common reasons for patient no-shows are distance, bad weather, fear, and discomfort of hospitals environment and privacy concerns. All these barriers can be eliminated with telehealth technology. And, this is a tried-and-tested conclusion.
The Ohio State University Wexner Medical Center experienced a reduction of 3% in missed appointments when the number of telehealth visits shot up from a modest 96 appointments in February 2020, to a whopping 202,900 virtual visits in July 2020.
The average cost of a telemedicine visit is much lower than an in-person visit. Let us explain how.
Firstly, hospitals and clinics don’t charge patients just for the consultation or the specific medical services that they are offering. They also charge for logistics, maintenance, cost of human resources, machines and equipment, etc. As discussed in the previous point, telemedicine significantly reduces these expenses for hospitals and diagnostic centers. This can, in turn, allow clinics to charge less from their patients. It’s a win-win for both parties.
Secondly, traveling expenses for face-to-face visits are the extra cost burden that we often don’t consider under medical expenditures. According to a report, patients in Ohio saved 9.2 million traveling miles and $830,000 fuel expense when they switched to telemedicine services post the Covid19 pandemic.
Thirdly, not all expenses are currency expenses. Time can also be factored in to money. Time wasted on traveling to a doctor’s clinic or waiting in the clinic, is, after all, a cost. This is called an ‘Opportunity Cost’. An interesting research done by the Harvard Medical School shows that during an ambulatory visit, an average adult spends a total of about 121 minutes for all the activities and this time roughly translates to an opportunity cost of $43 per adult which is actually higher than the out-of-pocket spending of $32.
Take a look at this amazing story boarding video by the Harvard Medical School to understand the opportunity cost:
Navigating telemedicine coverage is a perplexing aspect of this evolving healthcare delivery system. Rules vary between states and government or private payers. Reimbursement policies also differ across service types, encompassing store-and-forward methods, live video consultations, and remote patient monitoring (RPM). Within the list of pros and cons, this discrepancy stands as a prominent drawback, deterring providers from adopting these services.
No matter how hard we try, a technological interface cannot provide patients with the same seamless and organic experience as a face-to-face appointment. Sometimes, due to internet or network connectivity issues, the audio-visuals can get choppy or even completely freeze in the middle of a telemedicine video-consultation.
In other cases, people with hearing disabilities or light sensitivity can often find it difficult to communicate via a telemedicine interface.
Setting up telemedicine can be expensive, especially for small clinics and individual practitioners. Although the larger bulk of the expense is only a one-time investment, yet, the cost of purchasing high-tech hardware and software as well as paying for a high-speed internet connection might seem like an impractical misadventure to some.
Since Confy understands the pain points of your telemedicine goals, we believe in offering the most affordable telemedicine software solution packages.
A wide variety of telemedicine services and telemedicine software solutions are available in the market. Services can be delivered via mobile native apps or web applications .
A patient portal is like a registered personal account with a private dashboard showing every detail of patient activity and engagement to date. This information can include earlier appointments details, upcoming scheduled appointments, patient’s age, height, weight details, etc. Patients can also log-in to their portals and pay their providers through secure payment gateways.
A virtual waiting room is an interface within the telemedicine application that allows both patients and providers to wait in case their counterpart is delayed for the video conference. This is how a virtual wait works. The patient can log into their devices and see their doctor's status in real-time. If their physician is engaged in other appointments, it will be visible to the patients. Patients can utilize that wait time for other activities in-situ. Once the doctor is on board and is ready for live chat, the telemedicine application sends a notification signal to alert the patient. Patients can then click on a ‘JOIN NOW’ button and enter the live video-chat with their medical consultant.
A virtual waiting room works similarly at the provider’s end as well.
Telemedicine video-conferencing works just like any other video-conferencing app like Skype, Zoom, and Facetime that allows two-way audio-visual communication. However, since extremely sensitive and confidential data are shared during a telemedicine visit, telemedicine video-conference software solutions are required to be HIPPA-compliant to be considered as a legitimate medical service.
A digital prescription is a very convenient tool for providers. Physicians can directly type into the telemedicine application using a virtual keypad and once the virtual consultation is over, the digital prescription gets automatically updated on the patient’s dashboard. Patients can further download it and save it on their devices or share it with pharmacies or diagnostic centers. Besides, handwriting can often be hard to read. Thus, digital prescriptions are equally preferred by patients.
Advanced customizations can integrate a telemedicine application with a patient’s health and wellness gadgets like smartwatches, heart-rate monitoring devices, mobile step-counters, etc. This type of telemedicine software integration can be particularly useful for patients requiring super-special care (like quadriplegics, ALS-patients, etc.)
Paper-based medical records are very easily lost or damaged. Also, there is the inconvenience of scanning hard copies and sending them individually to different specialists in case of co-morbid health conditions. In such cases, advanced telemedicine software solutions can come to the rescue. Interoperability between the telemedicine software of different medical centers can be achieved to securely share patients’ medical data.
Telemedicine solutions are not the same for all. Therefore, it is crucial to decide beforehand what type of telehealth software solution you are looking for.
Before setting up a telemedicine program, providers and medical centers need to ask the three fundamental questions that we at Confy call the ‘P-B-S (Purpose-Budget-Scale) Basics’:
To get your complex questions on telemedicine solutions answered, read Confy's FAQ page or even better, interact with us!
Since healthcare is a state affair, telemedicine policy and procedures vary greatly across different states. This is particularly relevant in the case of reimbursement policies. Some states in the U.S. (like Arkansas, Delaware, Georgia, New Mexico, Utah, etc.) have telemedicine parity laws while other states don’t. Lack of pay-parity has often turned out to be a big deterrent for providers to jump into telemedicine practices.
The lack of regulatory uniformity in telemedicine negatively impacts physician licensing across state borders. If a specialist in one state aims to offer services to a patient in another state, the process isn't straightforward. Providers must adhere to regulations in both states, leading to potential confusion and conflicts. In the United States, tele-doctors who wish to routinely practice across state lines must hold a complete medical license for each state, which entails significant fees and extensive paperwork.
Another adverse by-product of having vague telehealth policies is the fear of getting sued for telemedicine malpractice. Telemedicine involves various security concerns and checkpoints which are not necessarily easy for providers to understand. This is often a big concern that medical practitioners face regarding telehealth programs.
The infrastructure for telemedicine is undoubtedly expensive. But on the brighter side, the lion’s share of the cost is only for the initial deployment of the telemedicine software and hardware. The ICT cost also varies across healthcare departments and medical specialties. For example, teleconsultation or teletherapy software solutions will cost much less than telesurgery or teleradiology infrastructures.
Telemedicine is a multi-disciplinary technology. What this means is that telemedicine software is built and maintained by IT professionals, used by healthcare professionals, and regulated by legal and governmental professionals. Therefore, the users of telemedicine platforms are expected to have a holistic idea about both the legal and technical aspects of Telehealth. This can only happen through proper training and education of the medical providers (doctors, nurses, etc.) Therefore, training can be an initial roadblock for providers as they often have a very hectic and tight schedule.
Much like any other change, the biggest barrier to the growth and development of the telemedicine industry is acceptance- acceptance from both patients and providers alike.
Many providers tend to resist using telemedicine as they strongly believe that they will not be able to deliver the same quality of care as an in-person visit and fear that it will result in their loss of reputation. Some healthcare professionals also feel that telemedicine may have privacy risks and ethical issues. However, one can hope that these irrational fears will gradually wear off, especially now that we have seen how useful and successful telemedicine programs can be post-Covid19.
HIPPA stands for Health Insurance Portability and Accountability Act of 1996. Institutionalized by the U.S. Department of Health and Human Services (HHS), the HIPPA sets a national standard of privacy rules and guidelines to safeguard electronic protected health information (e-PHI). The HIPPA act identifies several administrative, technical, and physical security protocols to ensure confidentiality, integrity, and availability of e-PHI.
The Office for Civil Rights (OCR) within the U.S. Department of Health and Human Services (HHS) is entrusted with the task of enforcing HIPPA.
There are two rules in place that act as tools to regulate HIPPA compliance for any healthcare activity dealt virtually or electronically (including telemedicine and telehealth activities). These are:
HIPPA compliance applies to both individuals and organizations dealing with electronic protected health information (e-PHI). Those who are required to comply with HIPPA guidelines are commonly referred to as HIPPA-covered entities. Covered entities can be furthered categorized as the following:
hospitals, clinics, doctors, nurses, pharmacies, etc.
A clearinghouse is an organization that converts health information on behalf of another organization (typically one that is directly involved in healthcare) to make them compliant with the mandated standards.
HMOs, insurance companies, government payers like Medicare, Medicaid, etc.
Furthermore, in the cases where covered entities include business associates in their healthcare activities, the business associate will also be required to comply with HIPPA privacy rules and HIPPA security rules.
Telehealth reimbursement and coverage policies are the most tricky and dynamic aspect of the telemedicine market. Unless there are telemedicine parity laws in a state, the payers often refuse to reimburse virtual visits the same way as an in-person visit.
Furthermore, telemedicine laws vary greatly by state. While some states have parity laws for only telemedicine video-conferencing (live telemedicine), others include store and forward telemedicine as well.
As if this wasn’t complicated enough, the telemedicine laws by states also vary in terms of coverage parity laws and reimbursement payment parity laws. Let’s understand the difference.
Therefore, Coverage Parity laws and Payment Parity laws are different in the context of the beneficiary involved.
Medicaid policies vary by state. Many states expanded coverage for telehealth services in response to the public health emergency. In fall 2022, the Center for Connected Health Policy (CCHP) reported that all 50 states and the District of Columbia had laws in place to ensure both coverage and payment parity for services.
At least 15 states in the United States have reimbursement payment parity laws. Utah and Washington passed parity laws in 2020, which will take effect from January 1, 2021. Besides these states, eight more states are also slated to implement telemedicine payment parity laws (according to the National Conference of State Legislatures).
Some states like Connecticut have coverage parity laws, but not payment parity laws.
You can know more about the detailed and updated state laws and reimbursement policies here.
Telemedicine payers can be of two types:
In the covid19 landscape, a number of these private payers in the telemedicine marketplace have updated their telemedicine and telehealth coverage policies. You can find them here
Currently, there are four major challenges of telemedicine.
Telemedicine suddenly came under the limelight post the global Coronavirus outbreak. Quarantine and social distancing norms pushed us indoors and made our laptops and mobile devices the sole conduit of communication. Hospitals and clinics became a scary place to step in to. Most of us have ditched physical visits and switched to virtual consultations since then.
Many of us hadn’t even heard of the name ‘Telemedicine’ before 2020 and now all of a sudden we are using it, searching the internet with questions like ‘what is telemedicine’ and ‘how to use telemedicine’. From this, one thing is clear: The world was in desperate need of this technology!
Now, before you roll your eyes and say that the growth of telemedicine will be over as soon as the world gets back to normal, let us show you a few telemedicine statistics and explain why your anticipation might be a little wrong.
Currently, South-east Asia, North America, and Australia are dominating the telemedicine market.
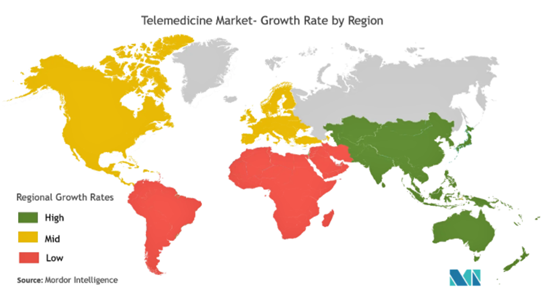 (Source: Mordor, 2020)
(Source: Mordor, 2020)
"Who nowadays would ever
use a bank that makes you come into a branch to access your money? Five
years from now, the question will be: Who is going to go to a doctor's office that makes you
come in every time you have the sniffles?"
- Jonathan Linkous, CEO, American Telemedicine Association
According to another Mckinsey report, approximately, $250 billion or 20% of total Medicare, Medicaid, commercial office visits, and home health expenditures could be virtualized.
The day is not very far when chatbots will tell us whether we need a face-to-face appointment with our doctors. Or, when, AI-powered telemedicine solutions will remind us of our medicines and doctor’s appointments. And no, this will not be under the special circumstance of a global pandemic or medical emergency. This will be the normal case. This will be the future of healthcare. The time has come to invest in telemedicine and the market leaders are already gearing up.
As already mentioned, Telemedicine is a collaborative sector. Software companies like Confy are the architects that silently work in the background to improve healthcare delivery. Our mission is to make medical care accessible to all and take the United Nation’s dream of Universal Health Coverage by 2030 one step further.
With Confy's White Label Program, you can even get your own unique telemedicine brand label.
Technology when used for the right purpose can create wonders and save lives. The world is constantly fighting pandemics and epidemics like the Ebola virus, Zika virus, and now Covid19. And yet, according to the World Health Organization, “at least than half of the world’s population still do not have full coverage of essential health services.” Telemedicine in the future will hopefully solve both the cost and accessibility pains of the current healthcare scenario.
HIPAA compliant and comprehensive solution to deliver quality virtual care to patients
Ask for Demo